How We Learn
What Makes Us Great
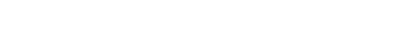
The University of Connecticut Orthopaedic Surgery Sports Medicine Fellowship Program aims to develop competent and professional orthopaedic surgeons, who are well prepared to join either private practice or academic medical centers. We provide exposure and opportunity in a wide variety of research activities including biomechanics, cell biology, outcomes, quality improvement, and patient safety. Our mission is to train inquisitive, talented surgeons dedicated to providing expert sports medicine care and increasing the fund of knowledge in our specialty. All of our faculty are extremely approachable and available for the needs of the fellows. Our block schedules afford us one-on-one teaching time with the fellows with little to no competition of residents which strengthens the fellows educational learning environment. At UConn we pride ourselves on mentorship and look forward to the lifelong relationships that are built between fellows and faculty.
Clinical Experience
Emphasis will be placed on the diagnosis and treatment of shoulder, elbow, hip, knee, ankle, and other sports injuries. These skills include:
- Focus on arthroscopic rotator cuff repair and biological as well as capsular augmentation, arthroscopic and open shoulder stabilization, elbow arthroscopy, arthroscopic and arthroscopic-assisted meniscal repair, cartilage and meniscal transplantation, and hip arthroscopy
- Exposure to complex reconstructive procedures including ACL, PCL and multiple ligament knee injury reconstruction and revisions, periarticular knee osteotomy, elbow reconstruction, total shoulder arthroplasty and reverse total shoulder arthroplasty
- Daily management of athletic injuries
- A complete rotation in pediatric and adolescent sports medicine, including pediatric and adolescent ACL reconstruction, making our program one of the most unique orthopaedic sports medicine training experiences in the world
The academic year is broken down into 2 month rotations in three different blocks. Two blocks take place at UConn Health and one at Connecticut Children’s. Fellows work one-on-one with assigned attendings in all aspects of patient care including:
- Outpatient Office: 2 days a week, on average
- Surgical Cases: 2-3 days a week, on average
- Training Room: 1 day a week, on average
Schedule
| Day | Fellow 1 | Fellow 2 |
| Monday | Coyner - Operating Room | Edgar - Operating Room |
| Tuesday | Arciero - Operating Room | Dwyer - Operating Room; Edgar - Clinic |
| Wednesday | Arciero - Clinic | Crepeau - Operating Room |
| Thursday | Coyner - Clinic | Edgar - Clinic |
| Friday | Research; Shea - Operating Room | Crepeau - Operating Room |
*Subject to change.
Didactics
The fellowship includes a robust didactic schedule including:
- Weekly: Sports medicine journal club
- Monthly: Cadaveric Bioskills Lab, MRI Indications Conference, and morbidity and mortality conferences
- Bi-monthly: Research meeting with Dr. Coyner
- Three Times Per Year: Grand rounds which feature a nationally or internationally known expert
UConn Orthopaedic residents and fellows with invited speaker, Dr. Thomas Byrd.
National Conferences
Fellows are resourced to attend several major orthopaedic meetings per year which include:
- Annual meeting of the American Orthopaedic Society for Sports Medicine
- Meeting of the New England Shoulder and Elbow Society
- Boston Shoulder Symposium
- Connecticut Orthopaedic Society Karen Zupko Coding Course
- West Point Fellows Day: Sports Medicine fellows from UConn Health, Keller Army Community Hospital, Hospital for Special Surgery, Lenox Hill Hospital, Columbia University, and New York University-Langone Medical Center exchange information and present new research during this unique regional conference
- Industry Sponsored Surgical Skills Courses (2-3 courses)
Bioskills Laboratory

Our Bioskills Laboratory is a fully operational, six-station lab with full-time support staff. Fellows use the lab to hone their technical skills and learn arthroscopic and other surgical procedures. During the dedicated bioskills lab once a month, faculty members demonstrate and practice arthroscopy and open surgical skills with the fellows. Fellows are able to repeat the demonstrated procedures on cadaveric shoulders, knees, and hips. In addition to formal monthly bioskills, the lab is available for additional training as desired. We have one of the first Virtual Reality surgical training modules.
The lab has full-size plasma screen monitors capable of projecting the arthroscopic views at the attending’s teaching station and surgical procedures taking place in our outpatient surgical center.
Fellows have immediate and direct access to the Musculoskeletal Institute's Bioskills Lab which provides a simulated surgical training facility with equipment similar to what is found in operating rooms. Fellows can also function as instructors in the laboratory for resident education to help build their teaching and mentoring skills. Equipment within the Bioskills Lab includes:
- Six work stations that contain suction, irrigation, and electrical power and can accommodate 24-30 residents/fellows
- Six arthroscopy towers with individualized monitors, arthroscopic shaver, and burrs
- Instrumentation and implantable devices to simulate both simple and complex sports medicine procedures arthroscopically, as well as open techniques
- Large C-arm with fluoroscopic capabilities
- Personal protective supplies including gloves, gowns, masks, and shoe covers
| Bioskills Schedule | |
| Month 1 | BTB ACL, practice quad harvest |
| Month 2 | RTC repair, subscapularis repair biceps tenodesis |
| Month 3 | Hip scope |
| Month 4 | Arthroscopic cappsolraphy and open Laterjet |
| Month 5 | HTO, DFO |
| Month 6 | TSA |
| Month 7 | MPFL and skeletally immature ACL |
| Month 8 | Elbow scope and distal biceps and UCL |
| Month 9 | Meniscal transplant and root repair |
| Month 10 | Hip scope |
| Month 11 | PCL graftlink and PCL and posteromedial corner reconstruction |
| Month 12 | Arthroscopic and open subscap repair |
On-Call Responsibilities
There is no on-call responsibilities besides covering call for the residents the night before the orthopaedic in-training examination.
Research Experience
Fellows will be provided ½ to one day per week, on average, for research. Opportunities exist for clinical, basic science, and translational research. Fellows are expected to complete three manuscripts during the year with an opportunity for additional research work as desired. There is support through research coordinators, medical editors, and statisticians. Fellows can make use of our world-class facilities, including the UConn Musculoskeletal Institute Human Cell and Tissue Biomechanics Lab which is equipped with:
- AC Rotation and Axial Fixture: we use this to investigate AC instability. The fixture can test for clavicle’s Horizontal (Ant-Post) and Rotation (Ant-Post) motions.
- Knee Simulator with 3D motion capture system which analyzes exact motion profile of the knee at various conditions: Used in knee related studies such as, testing tibial slope effects on ACL revision, MPFL and meniscal tear studies and studies involving osteotomies.
- Shoulder Simulator: Used to simulate shoulder motion with up to six actuators to mimic individual shoulder muscles, also complete with a 3D motion capture system.
Fellow research participation will be monitored through bi-monthly research meetings with the Director of Fellowship Research. Progress of each clinical and basic science project will be ascertained and aid in completion of all projects is facilitated. Fellows will each present their projects at the New England Shoulder and Elbow meeting in February, at the Annual Fellow’s Day at West Point Military Academy and at Fellowship Graduation.